HRT vs. birth control pills for perimenopause
Follows NC° Editorial Policy
At Natural Cycles, our mission is to empower you with the knowledge you need to take charge of your health. At Cycle Matters, we create fact-checked, expert-written content that tackles these topics in a compassionate and accessible way. Read more...
Key takeaways:
- Hormone therapy — also known as hormone replacement therapy or HRT — and birth control pills can both help manage perimenopause symptoms, but only birth control can prevent pregnancy
- Both hormone therapy and hormonal birth control can help protect your bones from osteoporosis and reduce the risk of certain cancers — but both have risks too.
- Choosing to start hormone therapy or take birth control to manage perimenopause is optional and should always be discussed with your doctor before beginning treatment
- Your choice will likely depend on your symptoms, health risks, and your contraceptive needs
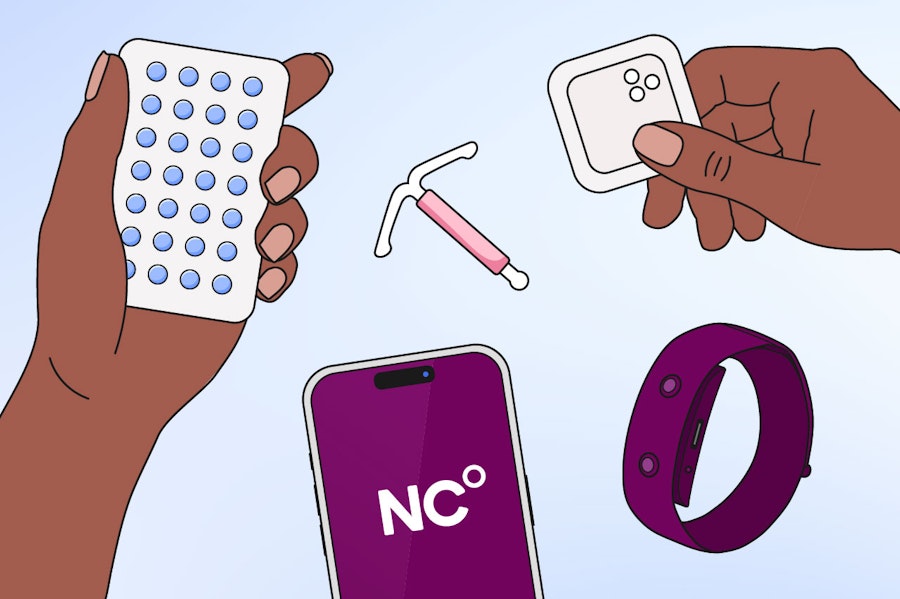
As we approach menopause, fluctuating hormones can cause uncomfortable symptoms, and many of us search for relief in hormonal treatments. But what is the difference between taking hormone therapy or the pill for perimenopause? In this article, we will look at the link between hormones and perimenopause, and the benefits and risks of both hormone therapy and birth control for symptom management.
The hormonal birth control and perimenopause connection
Many of us often hear or use the phrase “menopause” as a catchall term for the full transition. Though this is common, it is essential to understand the difference between perimenopause and menopause, particularly when thinking about hormonal birth control, as our contraceptive needs change during these distinct life phases.
Perimenopause refers to the years prior to menstruation ending and menopause being confirmed. Fluctuating hormones cause the start of menopausal symptoms, but you still have periods (even if they are irregular). The average age women begin perimenopause transition is 45-55, though some may experience it earlier. Menopause is the last menstrual period and is retrospectively determined when you have not had a period for over 12 months [1]. You then enter the phase after menopause, known as postmenopause.
During perimenopause, our levels of estrogen, progesterone, testosterone, and follicle-stimulating hormone (FSH) fluctuate in erratic ways we are not used to [2]. Though further research is needed, these varying hormone levels are thought to contribute to common perimenopause symptoms, such as [1]:
- Irregular periods
- Anxiety
- Brain fog
- Mood swings
- Hot flushes
- Night sweats
- Sleep problems
- Vaginal dryness
So what is the connection between perimenopause and hormonal birth control, like the pill? As age increases, the use of birth control generally declines [3]. But experiencing perimenopause does not mean you cannot get pregnant. If you have not had your uterus removed and you still have periods, there is still a chance that you might get pregnant, even if your periods are irregular. For those wanting to avoid pregnancy, contraception will still be necessary until menopause is confirmed.
Now, this is when an understanding of hormones comes in handy! Hormonal birth control has the potential to both protect from pregnancy and relieve some symptoms of perimenopause [4]. But it is not suitable for everyone, and you may wish to consider hormone therapy instead.
Hormone therapy vs. Birth Control
Hormone therapy is a treatment that traditionally provides estrogen, and usually progesterone, to replenish the natural loss of hormones as we age [5]. It is often also referred to as hormone replacement therapy or HRT. The most common treatment provided is a combination of both estrogen and progesterone. However, progesterone is only necessary to protect the uterus from extended estrogen exposure. For women who do not have a uterus, such as those who have had a hysterectomy, estrogen-only treatment can be prescribed. Hormone therapy can come in several forms, including oral tablets, transdermal patches, topical gels or creams, vaginal rings, and injections
Oral hormonal birth control is primarily taken as a contraception, also providing a combination of synthetic estrogen and progesterone (or sometimes progesterone-only). Combined birth control generally delivers stronger hormonal effects than hormone therapy, because it uses higher-potency synthetic hormones and doses sufficient to stop ovulation.
While both hormone therapy and birth control offer similar hormones, they also have their own advantages and disadvantages to consider. Lifestyle factors, medical history, and individual circumstances may mean one is more suited to you than the other. That’s why you should always speak to your healthcare provider before starting any hormonal treatment.
Hormone therapy for perimenopause: Benefits and drawbacks
The main benefit of hormone therapy is the relief of the most common menopause symptoms, such as night sweats, hot flushes, sleep problems, anxiety, mood swings, and vaginal dryness. But did you know there might be health benefits, too? Studies have shown that perimenopause is linked with loss of bone strength, beginning one to two years before reaching menopause [6, 7]. But hormone supplementation can help protect you from bone loss and reduce the risk of osteoporosis, as estrogen plays a vital role in maintaining healthy bones. In addition, hormone therapy can help maintain muscle strength as we age and may also reduce the risk of colon cancer [8, 9].
Like any medical treatment, hormone therapy does have some risks. These include a small increase in the risk of blood clots, stroke, and breast cancer, but the level of risk depends on the type of hormones used and how they are taken. For example, estrogen delivered through the skin, such as patches or gels, and forms that are closer to the body’s natural hormones tend to carry a lower risk of blood clots than oral estrogen because they enter the bloodstream directly rather than being processed by the liver first [10]. The choice of progesterone can also matter, as some types are better tolerated and may have fewer side effects [11].
Women who still have a uterus need to take progesterone along with estrogen to protect the lining of the uterus from cancer. Using estrogen alone can increase this risk. Because every woman’s health history is different, hormone therapy should always be personalized and discussed with your health practitioner. When the right hormones are matched to the right woman at the right time, the benefits usually significantly outweigh the risks, and serious side effects remain uncommon.
Hormonal birth control for perimenopause: Benefits and drawbacks
The most notable benefit of hormonal birth control over hormone therapy is the prevention of pregnancy. But there are health benefits, too. Both progesterone-only and combined birth control offer symptom relief from irregular or heavy periods and menstrual cramps, as well as other symptom relief similar to that of hormone therapy. Combined birth control can also reduce the risk of ovarian, endometrial, and colorectal cancers, and offers protection from bone loss [12].
Hormonal birth control can slightly increase the risk of blood clots, breast cancer, and heart-related problems. For most healthy people, these risks are small, but they can be higher in those who smoke, have high blood pressure, or have other health conditions. [4]. Progesterone-only birth control does not provide the same level of relief for common symptoms, such as hot flashes, as you may get with combined birth control or hormone therapy. As birth control can mask the symptoms of perimenopause, it may also make it difficult to spot the signs of perimenopause beginning and to confirm the occurrence of menopause [1].
Combining hormone therapy and birth control
If you are already using birth control, you may wonder if you should also be taking hormone therapy. The answer depends on the type of birth control you are using. Hormone therapy cannot be combined with any birth control containing estrogen (such as the combined pill), as this can cause an excess of estrogen. However, some progesterone-only birth control methods (like the IUD) may be used alongside estrogen-based hormone therapy. In certain cases, they can even provide the progesterone needed to protect the uterus, but this should be decided with your healthcare provider [8].
Many individuals who are taking combined birth control may also consider changing to hormone therapy. Choosing to switch is not for everyone, but it may be beneficial if contraception is no longer needed, or if lower-dose hormones are safer and more suitable for your stage of life.
Be sure to consult with your doctor before changing from birth control to hormone therapy, and do not take both at the same time without medical supervision.
How to use hormone therapy for perimenopause
There are a few different options when considering taking hormone therapy for perimenopause:
- Estrogen-only (transdermal, i.e., absorbed through the skin, or oral): Only suitable for women without a uterus, as progesterone is needed to protect the uterine lining from thickening, which can increase the risk of endometrial cancer [5]. You can take it as a pill, patch, gel, or spray.
- Estrogen-only (vaginally inserted): Used to treat localized vaginal symptoms, such as dryness or pain during sex. Available as a tablet, pessary, ring, gel, or cream.
- Progesterone/progestin-only*: Often recommended for addressing irregular or heavy periods, and only when there are no significant symptoms related to low estrogen, such as hot flashes or night sweats [13]. Available as a pill, implant, or IUD.
- Combined estrogen and progesterone/progestin: This type of hormone therapy includes both estrogen and progesterone (or a progestin). It is used for women who still have a uterus, as progesterone helps protect the lining of the uterus. The two hormones can be taken separately or together in a single pill or patch. Combined hormone therapy is the most commonly prescribed form of hormone therapy.
- Testosterone**: A hormonal gel only prescribed by a specialist to those in late perimenopause or postmenopause experiencing problems with sex drive or orgasm, when other treatments have not worked.
*Progesterone is a hormone produced naturally by the body, primarily in the ovaries. Progestins are synthetic compounds designed to mimic the effects of progesterone. You may be prescribed either, based on your individual needs and your doctor’s judgement.
**Testosterone is not FDA-approved in the United States for use in women but may be prescribed off-label by a specialist for postmenopausal women with persistent low sex drive (hypoactive sexual desire disorder) when other treatments have not been effective.
Stopping birth control in perimenopause
Choosing to stop birth control in perimenopause will depend on your personal circumstances, such as whether or not you are trying to get pregnant, your symptoms, and your health risks. Most guidelines recommend avoiding taking the combined contraceptive pill after age 50, and stopping contraception altogether at age 55 [1]. However, what is right for you may be different and will depend on your health, symptoms, and medical history. Similarly, whether or not you wish to use hormone therapy is an optional, and very personal, decision. There is no set time you must wait before you can begin taking it, either. Your doctor can help you choose the options that are safest and most appropriate for you.
If you do decide to come off hormonal birth control before perimenopause, you can use Natural Cycles as a hormone-free option to prevent pregnancy and track symptoms. For those who are already experiencing perimenopause, our new NC° Perimenopause option can be used to track symptoms and hormone use.
Note that Natural Cycles cannot be used to prevent pregnancy while using hormone therapy. If you’re not using hormone therapy or hormonal birth control, you can use Natural Cycles as an FDA-cleared birth control — simply log your temperature each day, and you’ll see a personalized fertility status in the app.
When to speak to a doctor
You should always speak with your doctor before starting any form of hormone therapy or hormonal birth control, as they may not be suitable if you:
- Have had, or currently have, breast cancer
- History of estrogen-based cancers
- Have had, or currently have, a blood clot or deep vein thrombosis
- Have cardiovascular disease or a high cardiovascular risk
- Have a high BMI
- Are a smoker
While this may seem like an exhaustive list, remember that there are many options of hormonal therapy available, and your risk factors are very individual. For example, transdermal estrogen (delivered via patches or gels) may be more suitable for those with a higher risk of blood clots or cardiovascular problems. Discuss your medical history and lifestyle with your doctor so they can recommend the most appropriate option for you.
Your symptoms make sense with Natural Cycles
A first step to understanding your body, perimenopause symptoms, and whether or not you wish to use hormone therapy is by tracking your cycle with Natural Cycles. You can record patterns and symptoms throughout your cycle, helping you visualize the changes you are experiencing, then bring them to your doctor to discuss your next steps. The app can be used to prevent pregnancy if you are coming off birth control, and if you are experiencing perimenopause, NC° Perimenopause can help you spot patterns, decode symptoms, and track hormone therapy use.
Did you enjoy reading this article?